 The terms bulging and herniated disc are often used interchangeably; however, many do not realize there are actually distinct differences between the two. While both impact the lumbar discs in our spine, bulging and herniated discs are not exactly the same.
The terms bulging and herniated disc are often used interchangeably; however, many do not realize there are actually distinct differences between the two. While both impact the lumbar discs in our spine, bulging and herniated discs are not exactly the same.
Here’s an overview of the key differences and similarities to help you better understand your condition and how you can address it.
Spinal Anatomy 101
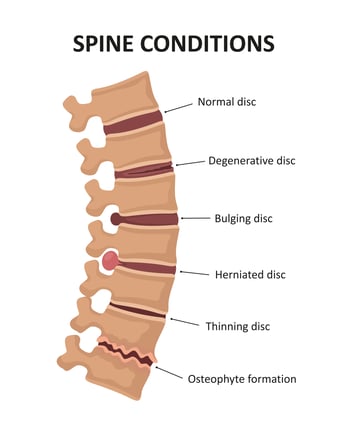
Before we discuss a bulging lumbar disc versus a herniated lumbar disc, it’s important to understand basic spine anatomy and the role our discs play in protecting the spinal cord. Our discs serve as cushions between the vertebrae (the bones) in the lumbar spine, protecting the spinal cord and acting as shock absorbers. Each disc has a soft, gel-like inner core called the nucleus pulposus and a thicker outer layer called the annulus fibrosus.
As we age, the discs in the lumbar spine naturally begin to dehydrate and stiffen, slowly showing signs of wear and tear—which is where bulging and herniated discs can come into play. Degenerative disc disease (DDD) is the most common cause of both bulging and herniated discs; however, they can also be caused by prolonged poor posture, excessive strain from heavy lifting, traumatic events resulting in injury, and certain hereditary conditions.
Either a bulging or herniated disc may result in compression of the spinal nerves. This compression can cause painful symptoms like leg pain (sciatica), tingling and numbness, and foot drop. Both bulging and herniated lumbar discs can also be present without causing pain or recognizable symptoms, which is dependent on the degree of degeneration and nerve compression.
Now that you have a better idea of how the discs function, let’s take a look at bulging lumbar discs and how they differ from herniated lumbar discs.
What Is a Bulging Lumbar Disc?
Sometimes referred to as disc prolapse, a bulging lumbar disc occurs when the soft inner nucleus pushes the annulus and “bulges” into the spinal canal but remains contained within the annulus. Despite the thick outer layer (annulus) of the disc remaining intact, this protrusion can cause some level of nerve compression. With that being said, disc bulges often occur within the aging process of the spine, and don’t always cause symptoms.
There are a few types of bulging lumbar discs that differ based on how much of the disc is affected. Asymmetric disc bulges typically impact 25-50 percent1 of the disc’s circumference. Additionally, a disc bulge is considered asymmetrical when it’s more severe on one side of the lumbar disc than the other.
The other type is a symmetric (or “circumferential”) disc bulge, which extends around the entire circumference of the lumbar disc. Symmetrical disc bulges occur when the right and left sides of the disc mirror each other. Regardless of whether the bulge is symmetric or asymmetric, it may be a sign that you’re in the early stages of degenerative disc disease.
 Stages of spinal osteochondrosis.
Stages of spinal osteochondrosis.
What Is a Herniated Lumbar Disc?
Herniated lumbar discs, which are also referred to as slipped or ruptured discs, occur when a hole in the outer layer (annulus) allows a piece of the gel-like core to protrude out of the disc (beyond the annulus) and commonly cause nerve compression. Disc fragments can also break off in a process called sequestration, compressing the spinal nerves and often causing painful symptoms.
Essentially, a bulging lumbar disc occurs during the earlier stages of degeneration, before herniation and sequestration transpire. In many cases, a bulging lumbar disc progresses into a herniated lumbar disc over time as degeneration becomes more advanced. The herniation can also occur from a traumatic event like a car crash, or by an overload like lifting heavy objects in an awkward position. While disc bulges often do not require treatment, herniated discs may need nonsurgical or surgical intervention for pain relief.
For many people, a lack of painful symptoms can make it difficult to catch a bulging lumbar disc soon enough to prevent it from advancing to the herniation stage. While disc bulges often do not require treatment, herniated discs may need nonsurgical or surgical intervention for pain relief.
Treating Herniated Lumbar Discs for Lasting Pain Relief
The best course of action is to take steps to lessen the risk of developing a bulging or herniated lumbar disc. However, if you already suspect you’re experiencing one of them, then the best way to differentiate between the two is to see a spine specialist for a physical exam and magnetic resonance imaging (MRI). By doing your research, meeting with a specialist, and exploring the best treatment options for you, you can find lasting relief from pain and discomfort.
While this blog is meant to provide you with information to support your well-being while considering or waiting for spinal surgery, it is not intended to replace professional medical care or provide medical advice. If you have any questions about the information given, please ask your doctor, who is the only one qualified to diagnose and treat your pain and spinal condition.
Reference:
1 David. F Fardon, MD, et al, "Lumbar disc nomenclature: version 2.0" The Spine Journal 14, no. 11 (2014): 2525-45, doi:10.1016/j.spinee.2014.04.022.



Comments