
Is your leg pain, cramping, numbness, and tingling keeping you up at night, off your feet during the day, and downright uncomfortable the majority of the time? If so, you may be suffering from a spine condition like a lumbar herniated disc or spinal stenosis.
Although a lumbar herniated disc and spinal stenosis can present a couple of similar symptoms, they’re very different conditions that require different treatment approaches. The first step to finding relief from unwelcome pain and limitations is to identify the condition that’s causing your discomfort. Only a physician can make that call, but here we try to provide an overview of the two conditions to help point you in the right direction.
Let’s compare a lumbar herniated disc versus spinal stenosis: what they are, common symptoms, risk factors, prevention techniques, and recommended treatments.
What is a lumbar discectomy?
A lumbar herniated disc occurs when a hole in the outer layer (the annulus) allows disc fragments to protrude outward, often compressing the spinal nerves and causing painful symptoms such as shooting leg pain (sciatica), tingling and numbness, and pain on the outer side of the foot due to spinal nerve root compression.
Protruding disc fragments can also break through the annulus and migrate away from the parent disc. In more severe cases, lumbar disc herniation can cause loss of bladder and/or bowel function, the feeling of “pins and needles” in the legs and/or feet, foot drop (difficulty lifting the foot), and pain that worsens with movement.
Causes of Lumbar Herniated Discs
Herniated discs are most commonly caused by degenerative disc disease (DDD), but can also result from certain lifestyle risks such as poor posture, excessive strain from heavy lifting, traumatic events resulting in injury, and some hereditary conditions.
While it’s not always possible to prevent a lumbar disc from herniating, there are certain steps you can take to minimize your risk, including:
- Maintaining good posture
- Quitting smoking/tobacco use
- Using proper lifting techniques
- Keeping a healthy weight
- Doing low-impact stretching
- Maintaining an active lifestyle
- Improving your core strength
Treatment of Lumbar Herniated Discs
Even if you can’t prevent lumbar disc herniation, it doesn’t have to be a permanent problem: More than 85 percent of patients with painful herniated discs see their symptoms resolve without surgery. Nonsurgical treatments like exercise and stretching, physical therapy, pain management, hot and cold therapies, and relaxation techniques can all help relieve your pain over time.
If nonsurgical treatments prove ineffective, your physician may recommend lumbar discectomy surgery to relieve uncomfortable symptoms. During lumbar discectomy surgery, a surgeon removes fragmented disc material to decompress spinal nerves and minimize associated pain. Your surgeon will recommend nonsurgical or surgical treatment, depending on your unique circumstances.
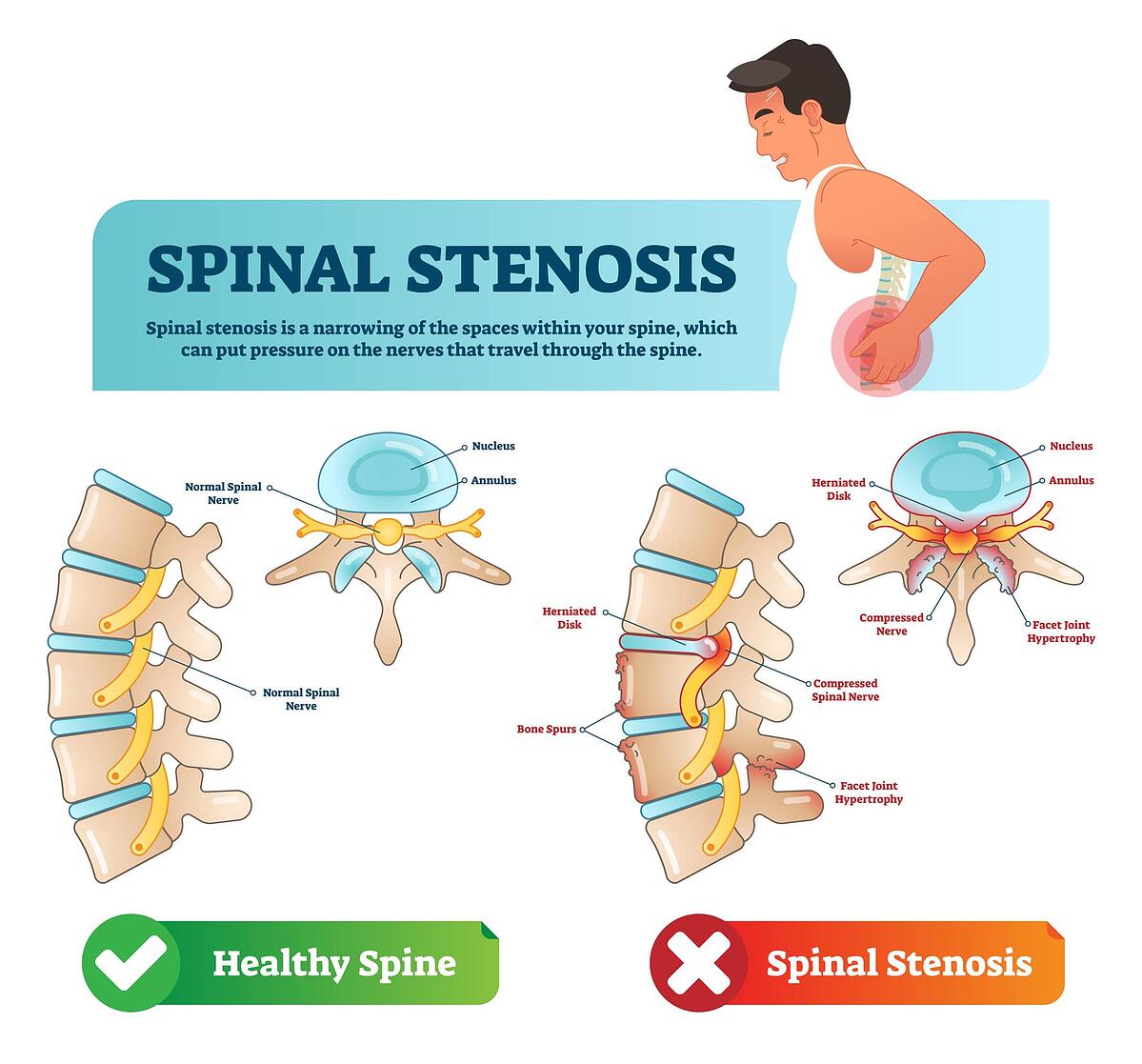
What is a lumbar spinal stenosis?
Lumbar spinal stenosis occurs when a patient’s spinal canal is more narrow than usual, which can put pressure on the spinal cord and surrounding nerves that travel through the spine, down the leg, and into the foot.
Some people with lumbar spinal stenosis don’t experience pain at all, but others experience symptoms that worsen over time, such as:
- Pain in the buttocks
- Pain in the lower back
- Muscle weakness
- Leg pain and cramping
- Numbness and tingling
- Loss of sensation in the legs/feet
Causes of Lumbar Spinal Stenosis
The cause of spinal stenosis can be categorized as either primary or acquired. Primary spinal stenosis is congenital and present at birth, occurring when people are born with a spinal canal that’s naturally too narrow. On the other hand, acquired spinal stenosis develops as a result of disease, injury, or natural degeneration.
Similar to a herniated disc, degenerative disc disease is a common cause of lumbar spinal stenosis due to the natural aging process. In fact, the symptoms of canal stenosis can be exacerbated by the presence of a herniated disc. Other causes of lumbar spinal stenosis include bone spurs, arthritis, spondylolisthesis, tumors, thickened ligaments, and scoliosis.
Treatment of Lumbar Spinal Stenosis
Although prevention and risk factors are similar for both conditions, the treatment approach differs in lumbar disc herniation and spinal stenosis. In addition to pain relievers, your physician may recommend tricyclic antidepressants or anti-seizure medications. Physical therapy and steroid injections at the site of the irritated nerve root can help reduce inflammation and relieve some pain.
If conservative treatments are ineffective, surgery may be recommended. Patients with lumbar spinal stenosis may be eligible for a decompression surgery, in which the surgeon will remove some bone and ligament to give more room for the nerves. Decompression may be performed via an endoscopic, minimally invasive, or open procedure. Alternatively, your physician may recommend a laminectomy and/or spinal fusion to treat spinal stenosis.
In the case of spinal stenosis worsened by a herniated disc, lumbar discectomy combined with laminectomy surgery is often the optimal approach.
Move forward with diagnosis and treatment.
If you’re experiencing any of the signs and symptoms of a lumbar herniated disc or lumbar spinal stenosis, consulting with a physician who specializes in spine conditions is the best next step. Diagnosing a herniated disc or spinal stenosis typically involves the combination of a physical exam, medical history review, and radiographic imaging such as x-rays, CT scans, and MRIs.
Imaging scans enable spine specialists to rule out other conditions and determine the specific pain type and location. Once you have a better understanding of which condition is causing your pain—as well as the likely root cause, whether congenital, degenerative, or otherwise—your physician can recommend the best treatment for you.
Relief is on the way—you just need to choose a qualified spine specialist to move forward with your diagnosis, answer any questions you may have, get started on treatment, and begin the healing process once and (hopefully) for all.
While this blog is meant to provide you with information you need to make an informed decision about your treatment options, it is not intended to replace professional medical care or provide medical advice.
The Barricaid device is designed to prevent reherniation following lumbar discectomy surgery. If you have any questions about the Barricaid, please call or see your doctor, who is the only one qualified to diagnose and treat your spinal condition. As with any surgical procedure, you should select a doctor who is experienced in performing the specific surgery that you are considering.
For additional information, please visit www.barricaid.com. For complete risk-benefit information: www.barricaid.com/instructions-for-use.
References
1 “Herniated Disk Prevention,” Cleveland Clinic, 2014, https://my.clevelandclinic.org/health/diseases/12768-herniated-disk/prevention.2 Alexander M. Dydyk et al, “Disc Herniation,” StatPearls, U.S. National Library of Medicine, 2021, https://www.ncbi.nlm.nih.gov/books/NBK441822.
3 “Spinal Stenosis,” Mayo Clinic, October 24, 2020, https://www.mayoclinic.org/diseases-conditions/spinal-stenosis/diagnosis-treatment/drc-20352966.


Comments