
For many years, discectomy surgery has remained the surgical gold standard for relieving chronic leg pain resulting from a herniated disc in the lumbar spine. In most cases, discectomy does exactly that; research shows that more than 80 percent1 of discectomy patients achieve good or excellent results after surgery.
There are different types of discectomy surgery, and this article compares aggressive versus limited discectomy surgery (i.e., how much of the disc nucleus is removed), highlighting the pros and cons of each option and an alternative approach that may be ideal for a subgroup of patients.
An Overview of the Types of Discectomy Surgery
When performing discectomy for lumbar disc herniation, your surgeon must determine how aggressive to be regarding disc fragment removal. The two types of discectomy surgery are aggressive and limited removal of disc material.
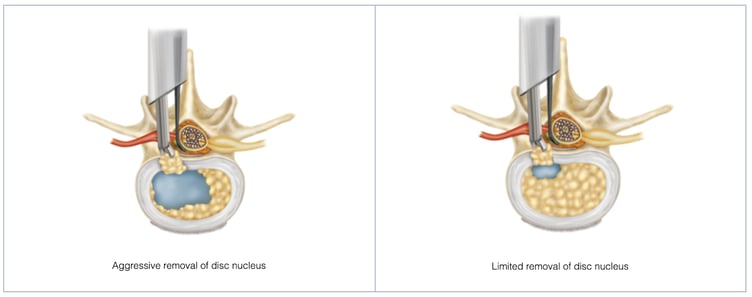
Aggressive discectomy involves removing all free disc fragments as well as additional material from inside the disc. Aggressive disc removal retains very little native disc nucleus and is thought to result in reduced reherniation rates2.
However, reherniation may still occur, and aggressive discectomy can also result in loss of disc height over time in comparison to a limited approach.Over time, loss of disc height can then cause some disc collapse, pain and stiffness.
During limited discectomy surgery (or “sequestrectomy”), the spine surgeon removes any free disc fragments from in and around the hole in the disc, without probing the nucleus pulposus (the inner core of the disc) or annulus fibrosus for additional disc material to remove.
Limited discectomy is a more conservative approach because it involves minimal invasion of the disc space. On one hand, limited disc removal has nearly double the risk of reherniation in comparison to the aggressive approach. On the other hand, disc collapse and associated back pain can be minimized, which may be a desired surgical strategy in patients that still have a rather healthy and tall disc, i.e. a disc worth saving.
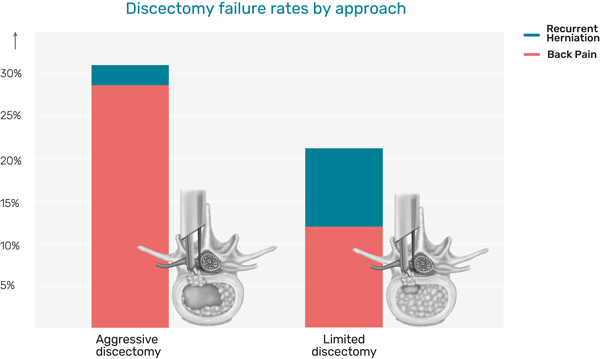
A study compares aggressive and limited discectomy failure rates
Reducing Reherniation with an Annular Closure Device
So, how will your surgeon determine the best approach for your discectomy surgery? The deciding factors include your spinal anatomy, the size of the hole in your annulus or outer ring of the disc, and your overall health.
Although the majority of discectomy patients see positive results after surgery, up to 18 percent3 experience reherniation and symptom recurrence. This often leads to the need for reoperation, which typically provides less favorable results than the initial discectomy surgery. In fact, multiple studies found that clinical outcomes are worse4 for patients who must undergo reoperation.
Certain patients are at higher risk5 of recurrent lumbar disc herniation after discectomy. Individuals with large annular defects (6mm wide and larger) face 2.5 times6 the risk of reherniation compared to other discectomy patients, when treated with a limited discectomy. Some of the other known risk factors for reherniation after discectomy surgery include obesity, tobacco use, diabetes, inactivity, and playing high-impact sports like football.
The good news is, thanks to breakthrough medical and technological advancements, there is a new and well-researched treatment pathway to explore.
Limited Discectomy with Barricaid
Many high-risk patients (primarily those with a large defect in their disc) benefit from implantation of an annular closure device which has been shown to reduce their reherniation risk following discectomy surgery. This innovation aims to help high-risk patients significantly decrease their chance for a reherniation and reoperation.
 Firmly anchored Barricaid device holding back nucleus and closing annular hole
Firmly anchored Barricaid device holding back nucleus and closing annular hole
Implanting the Barricaid device allows the surgeons to access the potential benefits of limited discectomy and remove less disc nucleus in order to help maintain disc height, while also closing the hole in the annulus. This provides the option to preserve native disc nucleus material which may help maintain disc height, while effectively reducing the risk of reherniation and the need for repeat surgery. Reherniation risk is substantially lower with implantation of the Barricaid device, although still not reduced to zero.
Barricaid is designed to withstand the enormous amount of pressure inside of a disc; in fact, up to 330 pounds per square inch of pressure or 10 times7 the pressure in a standard car tire. Clinical evidence8 shows that implanting the Barricaid reduces symptomatic recurrent disc herniation by 50 percent and associated reoperations by 60 percent. Like with all medical devices there are risks associated with the Barricaid device. For complete risk-benefit information: www.barricaid.com/instructions-for-use.
Explore the Options with Your Surgeon
If you’re considering a discectomy to relieve chronic leg pain from a herniated disc, it’s important to know the different treatment options and why one in particular might be a better fit for you than others. Your spine surgeon can make the final determination during surgery regarding whether or not you can benefit from a Barricaid device based on the size of your annular defect.
Discuss the option with your surgeon prior to the procedure to learn more about the types of discectomy surgery and which surgical approach is an ideal fit for you. In the meantime, you can take our free candidate quiz to learn whether or not you’re a likely candidate for the Barricaid device.
While this blog is meant to provide you with information to support your well-being while considering or waiting for spinal surgery, it is not intended to replace professional medical care or provide medical advice. If you have any questions about the information given, please ask your doctor, who is the only one qualified to diagnose and treat your pain and spinal condition.
If you have any questions about Barricaid, you may ask your doctor. For additional information, please visit www.barricaid.com. For complete risk-benefit information: www.barricaid.com/instructions-for-use.
References:
1 George J. Dohrmann and Nassir Mansour, “Long-Term Results of Various Operations for Lumbar Disc Herniation: Analysis of Over 39,000 Patients,” Med Princ Pract 24, no.3 (2015): 285-290, doi: 10.1159/000375499.
2 Eugene J. Carragee et al, "A Prospective Controlled Study Of Limited Versus Subtotal Posterior Discectomy: Short-Term Outcomes In Patients With Herniated Lumbar Intervertebral Discs And Large Posterior Annular Defect," Spine 31, no. 6 (2006): 653-657, doi:10.1097/01.brs.0000203714.76250.68.
3 Ibid.
4 Dante Leven et al, "Risk Factors For Reoperation In Patients Treated Surgically For Intervertebral Disc Herniation," The Journal Of Bone And Joint Surgery-American 97, no. 16 (2015): 1316-1325, doi:10.2106/jbjs.n.01287; Jeffrey A O’Donnell et al, "Treatment Of Recurrent Lumbar Disc Herniation With Or Without Fusion In Worker’s Compensation Subjects," Spine 42, no. 14 (2017): E864-E870, doi:10.1097/brs.0000000000002057; Junyoung Ahn et al, "Primary Versus Revision Single-Level Minimally Invasive Lumbar Discectomy," Spine 40, no. 18 (2015): E1025-E1030. doi:10.1097/brs.0000000000000976.
5 Larry E. Miller et al, “Association of Annular Defect Width After Lumbar Discectomy With Risk of Symptom Recurrence and Reoperation: Systematic Review and Meta-Analysis of Comparative Studies,” Spine 43, no. 5 (2018): E308-E315, doi: 10.1097/BRS.0000000000002501.
6 Larry E. Miller et al, “Association of Annular Defect Width After Lumbar Discectomy With Risk of Symptom Recurrence and Reoperation: Systematic Review and Meta-Analysis of Comparative Studies,” Spine 43, no. 5 (2018): E308-E315, doi: 10.1097/BRS.0000000000002501.
7 H.J. Wilke et al, “New in Vivo Measurements of Pressures in the Intervertebral Disc in Daily Life,” Spine 24, no. 8 (1999): 755-762, doi: 10.1097/00007632-199904150-00005.
8 Claudius Thomé et al, “Annular closure in lumbar microdiscectomy for prevention of reherniation: a randomized clinical trial,” The Spine Journal 18 (2018): 2278-2287, doi: 10.1016/j.spinee.2018.05.003.


![[You may be able to decrease your chance of a repeat herniation after your first discectomy by 50%. Take this quiz to find out.]](https://no-cache.hubspot.com/cta/default/7330018/10ff7b73-96e0-4fa7-919b-f4b5430bd91b.png)
Comments