Can a Microdiscectomy Treat Spinal Stenosis Effectively?
For people who are dealing with back pain and nerve symptoms, understanding the difference between various spinal conditions and their treatments can be overwhelming. Two conditions that often cause confusion are herniated discs and spinal stenosis. While both involve the spine and can cause similar symptoms, they represent different conditions requiring different treatment approaches.
Herniated discs are the most common reason microdiscectomy is performed, while spinal stenosis is a condition characterized by narrowing of the spinal canal. In this article, you will gain a better understanding of whether microdiscectomy can help with spinal stenosis and what treatment options are most appropriate for each condition.
Understanding Microdiscectomy: What It Is and How It Works
Microdiscectomy is a minimally invasive surgical procedure specifically designed to treat herniated or bulging discs in the spine. During this procedure, surgeons remove portions of the herniated disc material that is pressing on spinal nerves, thereby relieving pain and other neurological symptoms.
The procedure involves making a small incision, typically 2.5 to 5 centimeters long, in the skin over the affected area. The surgeon then removes a small portion of the lamina (the bone forming a roof over the spinal canal) and sometimes part of the facet joint to access the herniated disc material. Unlike traditional open surgery, microdiscectomy preserves most of the surrounding bone and muscle tissue, leading to faster recovery times and reduced surgical trauma.
Research indicates microdiscectomy has a significant success rate as treatment for herniated discs. Studies suggest approximately 84 percent of patients who undergo microdiscectomy experience long-term success in treating their herniated disc symptoms. The procedure is particularly effective for patients experiencing sciatica, a painful condition caused by compression of the sciatic nerve due to disc herniation.
What Spinal Stenosis Involves
Spinal stenosis is a condition characterized by the narrowing of the spinal canal or intervertebral foramina. This narrowing can occur in various parts of the spine but most commonly affects the lumbar (lower back) and cervical (neck) regions.
Unlike disc herniation, which involves the displacement of disc material, spinal stenosis typically results from age-related changes in the spine, including thickening of ligaments, bone spurs, and general wear and tear on spinal structures. The narrowed space can compress the spinal cord or nerve roots, leading to pain, numbness, weakness, and other neurological symptoms.
The symptoms of spinal stenosis can be similar to those of disc herniation, including leg pain, low back pain, and neurological symptoms. However, the underlying cause and optimal treatment approaches differ significantly between these two conditions.
The Relationship between Microdiscectomy and Spinal Stenosis
The critical question many patients ask is whether microdiscectomy can help with spinal stenosis. The answer is nuanced and depends on the specific circumstances of each case.
Microdiscectomy is not typically the primary treatment for spinal stenosis because the procedures target different underlying problems. Microdiscectomy removes herniated disc material, while spinal stenosis requires decompression of the narrowed spinal canal through different surgical techniques.
However, there are situations where these conditions can coexist. Some patients may have both a herniated disc and spinal stenosis simultaneously. In such cases, addressing the herniated disc through microdiscectomy may provide partial relief, but it may not fully resolve symptoms caused by the underlying stenosis.
Surgical Options for Spinal Stenosis
When conservative treatments fail to provide adequate relief for spinal stenosis, several surgical options are available, each designed to address the specific anatomy causing nerve compression:
Laminectomy
Laminectomy involves removing part or all of the lamina to create more space for the spinal cord and nerves. This procedure directly addresses the narrowing characteristic of spinal stenosis by enlarging the spinal canal.
Laminotomy
A less invasive option than full laminectomy, laminotomy involves removing only a portion of the lamina to relieve pressure on specific nerve roots while preserving more of the spinal structure.
Foraminotomy
This procedure focuses on enlarging the foramina (openings where nerve roots exit the spinal canal) to relieve pressure on compressed nerves.
Endoscopic decompression
Recent advances in minimally invasive techniques have led to endoscopic approaches for treating spinal stenosis. Research comparing full-endoscopic versus microscopic spinal decompression has shown that both techniques are safe and effective for treating symptomatic lumbar spinal stenosis, with clinically comparable results.
When Both Conditions Coexist
In clinical practice, some patients present with both disc herniation and spinal stenosis. This combination can complicate treatment decisions and may require a more comprehensive surgical approach.
When both conditions are present, the surgeon may perform a combination of procedures during the same operation. For example, the surgeon might perform a microdiscectomy to address the herniated disc while also conducting decompressive procedures to address the stenosis. The specific approach depends on the severity of each condition and the patient’s overall symptom profile.
Recovery and Long-Term Considerations
Recovery from spinal surgery varies depending on the specific procedure performed and individual patient factors. Microdiscectomy typically involves a shorter recovery period compared to more extensive decompressive surgeries for spinal stenosis.
Patients undergoing microdiscectomy often experience faster pain relief compared to nonsurgical treatment options. However, research indicates about 5 to 15 percent of patients may experience recurrent disc herniation, either at the same location or on the opposite side.
For patients with spinal stenosis, recovery may take longer, particularly if more extensive decompressive procedures are required. The long-term success of stenosis surgery depends on various factors, including the extent of narrowing as well as the patient’s age and overall health status.
Making the Right Treatment Decision
Determining whether microdiscectomy or other surgical interventions are appropriate requires comprehensive evaluation by qualified spine specialists. The decision-making process should include:
Accurate diagnosis
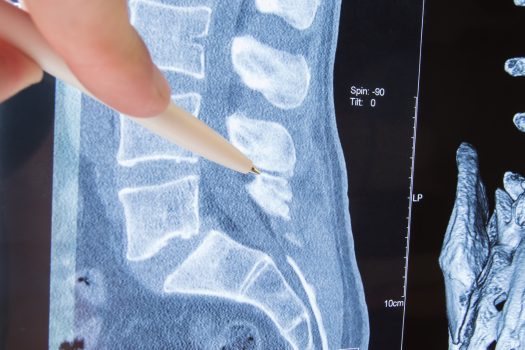
Advanced imaging studies, including MRI and CT scans, are essential for distinguishing between disc herniation and spinal stenosis. These studies help doctors identify the specific anatomical problems contributing to symptoms.
Conservative treatment trial
Most spine conditions benefit from an initial trial of conservative treatments, including physical therapy, medications, and epidural injections. Surgery is typically considered only after conservative approaches fail to provide adequate relief.
Surgical risk assessment
Each patient’s surgical risk profile must be carefully evaluated, considering factors such as age, overall health, and the specific anatomy involved.
Expected outcomes
Realistic expectations about surgical outcomes should be discussed, including potential benefits, risks, and the possibility that additional treatments may be needed in the future.
While microdiscectomy is not a direct treatment for spinal stenosis, understanding the relationship between different spinal conditions is crucial for patients and healthcare providers. Microdiscectomy specifically addresses herniated disc material, while spinal stenosis requires different surgical approaches focused on decompressing the narrowed spinal canal.
The key to successful treatment lies in accurate diagnosis, appropriate patient selection, and choosing the right surgical technique for the specific underlying problem. Patients experiencing back pain and neurological symptoms should work closely with qualified spine specialists to determine the most appropriate treatment approach for their individual situations.
As surgical techniques continue to advance, patients have access to increasingly sophisticated and minimally invasive options. However, the fundamental principle remains the same: matching the right treatment to the right condition is essential for optimal patient outcomes.
Although microdiscectomy surgery is generally a very successful procedure, a hole is left in the outer wall of the disc. In fact, patients with these large holes in their discs are more than twice as likely to reinjure themselves by having what is known as a reherniation. These reherniations often require additional surgery or even fusions. Fortunately, there is a new treatment specifically designed to close the large holes that are often left in spinal discs after discectomy surgery. Barricaid is a bone-anchored device proven to reduce reherniations, and 95 percent of Barricaid patients did not undergo a reoperation due to reherniation in a 2-year study timeframe. This treatment is done immediately following the discectomy—during the same operation—and does not require any additional incisions or time in the hospital.
If you have any questions about the Barricaid treatment or how to get access to Barricaid, ask your doctor or contact us today.
For full benefit/risk information, please visit: https://www.barricaid.com/instructions.


Comments