Understanding Discectomy with Annuloplasty: Procedure, Benefits, and Recovery
Spinal disc herniation is a prevalent cause of lower back and leg pain, especially among adults aged 30 to 50. Traditional discectomy procedures aim to relieve nerve compression by removing herniated disc material. However, discectomy alone does not address the annular tear, a weakness in the outer ring of the disc that often precedes herniation. This has led to the evolution of discectomy with annuloplasty, a technique that repairs both the herniation and the damaged annulus fibrosus, aiming for long-term relief and reduced risk of recurrence.
This combined procedure has gained prominence as spine surgeons seek more comprehensive solutions for disc-related conditions while minimizing surgical trauma and recovery time. Here we’ll explore in more depth what discectomy with annuloplasty entails, how it differs from standard discectomy, who may benefit, and what clinical studies say about its outcomes.
Understanding the Anatomy: Why This Procedure Is Necessary
The intervertebral disc consists of two primary components: the nucleus pulposus (the gel-like center) and the annulus fibrosus (the tough outer ring). When the annulus develops tears or weakens, it can allow the nucleus pulposus to leak out, or herniate, creating pressure on nearby nerves and causing pain. Traditional discectomy addresses the herniated material but often leaves the annular defect unrepaired, potentially leading to recurrent herniation.
The combination of discectomy with annuloplasty specifically targets both issues. The discectomy component removes the problematic disc material that is compressing nerves, while the annuloplasty addresses the structural weakness in the disc wall that allowed the herniation to occur initially. This dual approach aims to provide more comprehensive treatment and potentially reduce the risk of reherniation.
Discectomy Explained
A discectomy is a surgical procedure that removes the herniated portion of a spinal disc. It can be performed through traditional open surgery or minimally invasive techniques like microdiscectomy, which uses a microscope for better visualization through a smaller incision.
During the discectomy, the surgeon carefully removes the problematic disc material while preserving as much healthy tissue as possible. This selective removal maintains the structural integrity of the disc while eliminating the source of nerve compression. While it is effective at relieving nerve pressure, discectomy by itself does not always address the root structural issue: the torn annulus. This may lead to reherniation in a small but significant percentage of cases.
Understanding Annuloplasty
Annuloplasty is a therapeutic technique that repairs or strengthens the annulus fibrosus, the outer ring of the intervertebral disc. The procedure typically involves the application of controlled thermal energy to the damaged annular tissue. This thermal treatment serves multiple purposes: it can seal tears in the annulus, reduce pain-generating nerve fibers within the disc, and potentially strengthen the disc wall to prevent future herniation. In addition, a closure device (such as Barricaid) may be implanted to close the hole in the annulus.
The Combined Procedure: How Discectomy with Annuloplasty Works
When performed together, discectomy with annuloplasty creates a comprehensive treatment approach. This surgery, done through a tiny opening in the skin, typically follows these steps:
- Using fluoroscopic guidance, the surgeon inserts a needle through the skin and advances it to the affected disc. A guide wire is then placed through the needle, and the needle is removed. A tapered cannula is advanced over the guide wire to create a working channel to the disc space.
- Through this cannula, an endoscope is inserted, allowing direct visualization of the disc interior. The surgeon first performs the discectomy, removing herniated or degenerated disc material that is causing nerve compression.
- Following the discectomy, the annuloplasty component begins. A specialized radiofrequency probe is introduced to deliver controlled thermal energy to the annular tears and surrounding tissue.
Clinical Indications and Patient Selection
Discectomy with annuloplasty is indicated for specific patient populations and conditions, and it generally results in a notable reduction in leg pain, back pain, and disability within a few days to months after the surgery.
The procedure is typically considered for patients with:
- Lumbar disc herniation with radicular symptoms that have not responded to conservative treatment
- Combined disc herniation with significant annular tears
- Discogenic back pain associated with annular disruption
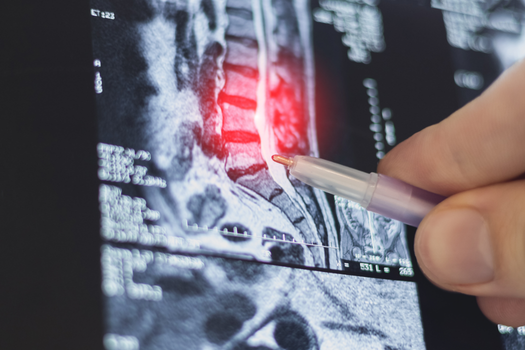
Patient selection requires careful evaluation of imaging studies, symptoms, and response to conservative treatments. Magnetic resonance imaging (MRI) is essential to assess the degree of disc herniation, the presence and extent of annular tears, and the overall condition of the affected disc. Additionally, patients should have realistic expectations about outcomes and understand that while the procedure can be highly effective, it may not completely eliminate all symptoms.
Clinical Outcomes and Effectiveness
Research demonstrates promising outcomes for discectomy with annuloplasty procedures. Studies have shown significant improvements in pain scores, functional outcomes, and quality of life measures. This procedure has been reported to be an effective treatment for discogenic low back pain, particularly in specific patient populations. Research involving elite athletes has shown particularly encouraging results, with patients experiencing significant pain reduction and successful return to high-level athletic activities.
According to additional studies, patients receiving annular closure in addition to discectomy have lower rates of reherniation. For example, one study demonstrated that use of an annular closure device significantly reduced the need for revision surgery compared to discectomy alone.
These findings suggest the combined approach may offer advantages over either procedure performed alone. The timeline for improvement varies among patients, with some experiencing relief within days, while others may require several months to achieve maximum benefit. The multifactorial nature of disc-related pain means outcomes can be influenced by various factors, including the degree of disc degeneration, patient age, activity level, and concurrent conditions.
Potential Risks and Complications
While discectomy with annuloplasty is generally considered safe, patients should be aware of potential risks and complications. Those risks include, but are not limited to, increased pain, bleeding, and infection. In general, an annuloplasty procedure is very safe, and serious side effects or complications are rare.
The thermal component of annuloplasty carries specific risks related to heat application, including the potential for thermal injury to nerve structures or excessive tissue damage if temperatures or duration exceed safe parameters. The risks are generally lower than with open surgical procedures, but patients should discuss all potential risks with their surgeons before proceeding.
Recovery and Postoperative Care
Recovery from discectomy with annuloplasty typically follows a structured protocol designed to optimize healing while preventing complications. Immediate postoperative care focuses on monitoring for any signs of complications and managing pain effectively. Most patients experience some degree of local soreness at the procedure site, which is normal and expected.
Activity restrictions in the initial recovery period usually include avoiding heavy lifting, prolonged sitting, and high-impact activities. Patients are typically encouraged to walk and perform light activities as tolerated while avoiding movements that could stress the treated disc. Physical therapy may be recommended to restore function and prevent future problems.
The recovery timeline varies among individuals, but many patients report significant improvement in symptoms within the first few weeks following the procedure. Full recovery and return to normal activities typically occurs over several months as the treated tissues heal and strengthen.
Future Directions and Innovations
The field of minimally invasive spine surgery continues to evolve, with ongoing research into improved techniques for discectomy with annuloplasty. Reconstruction of the fibrous ring defect is currently one of the promising areas in preventing recurrent lumbar disc herniation. New technologies and materials are being developed to enhance the effectiveness of annular repair and potentially provide longer-lasting results. Advances in imaging technology, surgical instruments, and biomaterials may further improve outcomes and expand the applicability of these procedures.
Discectomy with annuloplasty represents a sophisticated approach to treating disc herniation and discogenic pain that addresses both the immediate problem and underlying structural damage. This procedure offers patients an alternative to more extensive open surgery while providing comprehensive treatment of disc-related conditions. While outcomes are generally favorable, success depends on appropriate patient selection, skilled surgical technique, and comprehensive postoperative care. Patients considering this procedure should discuss their specific situations with qualified spine specialists to determine if discectomy with annuloplasty is appropriate for their condition.
Even though a discectomy is a common and generally quite successful procedure, a hole is frequently left in the outer wall of the disc. In fact, patients with these large holes in their discs are more than twice as likely to reinjure themselves by having what is known as a reherniation. These reherniations often require additional procedures or even spinal fusion surgery. Fortunately, there is a new treatment specifically designed to close the large holes that are often left in spinal discs after discectomy surgery. Barricaid is a bone-anchored device proven to reduce reherniations, and 95 percent of Barricaid patients did not undergo a reoperation due to reherniation in a 2-year study timeframe. This treatment is performed immediately following the discectomy—during the same operation—and does not require any additional incisions or time in the hospital.
If you have any questions about the Barricaid treatment or how to get access to Barricaid, ask your doctor or contact us today.
For full benefit/risk information, please visit: https://www.barricaid.com/instructions.


Comments