 Discectomy surgery has been considered the surgical gold standard for relieving sciatica symptoms resulting from a herniated disc in the lumbar spine, in cases when conservative treatment doesn’t work. Research reveals that 84 percent1 of lumbar discectomy patients achieve either good or excellent results following surgery. With that said, there are different approaches to lumbar discectomy surgery, and determining the best fit for you is imperative in order to yield successful results.
Discectomy surgery has been considered the surgical gold standard for relieving sciatica symptoms resulting from a herniated disc in the lumbar spine, in cases when conservative treatment doesn’t work. Research reveals that 84 percent1 of lumbar discectomy patients achieve either good or excellent results following surgery. With that said, there are different approaches to lumbar discectomy surgery, and determining the best fit for you is imperative in order to yield successful results.
Although only a qualified spine surgeon can make a recommendation on the best surgical technique, doing your research and knowing your options in advance will empower you to make a fully informed decision regarding your treatment plan. In this article, we’ll define and compare the different minimally invasive discectomy techniques for treating a lumbar herniated disc.
What is minimally invasive spine surgery (MIS)?
In recent years, surgeons have moved toward minimally invasive spine procedures in the hopes of reducing recovery time, improving patient outcomes, and minimizing complications. Technology is available to magnify and transmit images, resulting in different MIS approaches such as lumbar microdiscectomy, lumbar micro tubular discectomy, and lumbar percutaneous transforaminal endoscopic discectomy.
In comparison to open spine surgery, MIS procedures may be safer, faster, and easier to recover from. Although the benefits of MIS over "open" discectomy are moderately controversial, the rationale behind choosing the minimally invasive route is that a smaller incision could result in:
- Reduced risk of infection and postoperative pain
- Less reliance on pain medication after surgery
- Better cosmetic results (smaller incision and less scarring)
- Potential for less blood loss during surgery
- Reduced risk of damage to the muscles
Are there different types of lumbar discectomy surgery?
The different types of lumbar discectomy surgery include the following:
Open Lumbar Discectomy
Open discectomy is the most established surgical treatment for lumbar herniated disc pain relief. Unilateral transflaval discectomy is the most common “open” procedure, and it has become the preferred surgical approach for treatment of patients with symptomatic lumbar disc herniation, to which all other techniques should be compared.
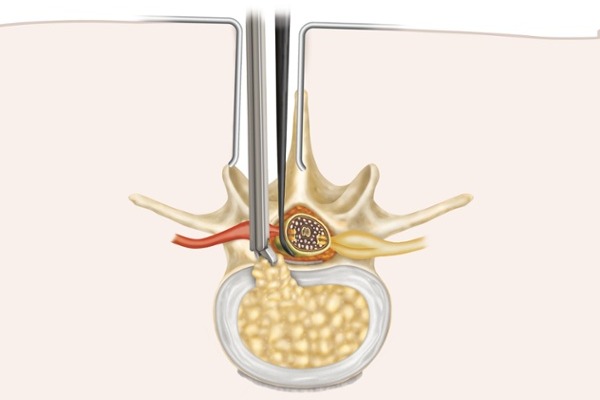
During an open discectomy, the spine surgeon makes an incision along the midline of the lower back, gently pushes overlying muscles to the side, and removes lamina (laminectomy) as needed. After the nerve root is gently moved aside, the surgeon uses small instruments to remove herniated disc fragments. Unlike the other approaches to discectomy surgery, open procedures do not involve the use of a microscope or loupes (special eyeglasses) for greater visual enhancement.
Open discectomy is favored by many surgeons due an abundance of published research on clinical outcomes, direct visualization and lower instrumentation costs, and less of a surgical learning curve because it doesn’t require the use of emerging technology, there’s less of a learning curve for surgeons performing the procedure.
Lumbar Microdiscectomy
A lumbar microdiscectomy is performed through the back using a small incision near the midline of the lower back. Lumbar microdiscectomy allows for a smaller incision than open discectomy, but it may also require a laminectomy for better access.
During a microdiscectomy, a spine surgeon uses a microscope or loupes to clearly see the compressed nerve root that’s causing pain and discomfort. This is the key difference between open discectomy and microdiscectomy. Then, a lumbar microdiscectomy follows the same process as open discectomy, using a small instrument to remove herniated disc fragments.
As lumbar microdiscectomy becomes the new surgical standard, it’s now being considered equally effective compared to open procedures because it involves a smaller incision and less blood loss, fewer side effects, and fewer complications than lumbar open discectomy. The learning curve is also fairly minimal, as more spine surgeons become more comfortable with the microdiscectomy approach. In some cases, lumbar microdiscectomy may lead to more blood loss than a lumbar micro tubular discectomy.
Micro Tubular Discectomy (MTD)
Micro tubular discectomy can be effective, but has a steep learning curve because it requires expert recognition of anatomy and use of instruments. Studies2 comparing tubular discectomy with microdiscectomy for treatment of sciatica resulting from lumbar disc herniation point to an increased risk of complications and less favorable outcomes for the tubular approach. This is likely due to a steep learning curve, because many spine surgeons are still unfamiliar with micro tubular discectomy.
Percutaneous Transforaminal Endoscopic Discectomy (PTED)
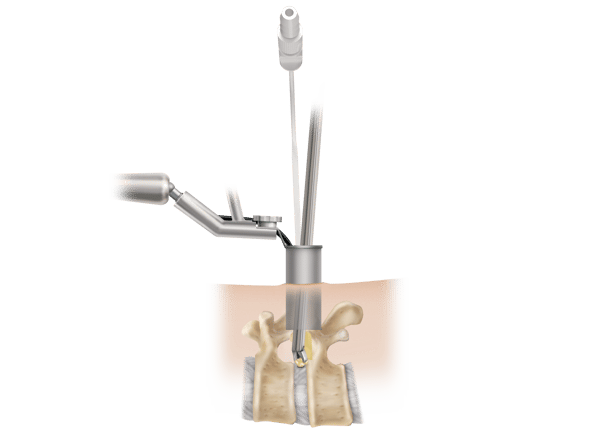
.png?width=600&name=Endoscopic-Lumbar-decompression%20(1).png) Lumbar percutaneous transforaminal endoscopic discectomy is another minimally invasive procedure, which also involves a smaller incision than open discectomy and the use of an endoscope for better visualization. Using the endoscope—a special optical instrument with a tiny camera attached that’s used as a viewing system for examining areas deep inside the body—a surgeon can get a precise look at the spinal discs, herniated disc fragments, and nerve roots in the lumbar spine.
Lumbar percutaneous transforaminal endoscopic discectomy is another minimally invasive procedure, which also involves a smaller incision than open discectomy and the use of an endoscope for better visualization. Using the endoscope—a special optical instrument with a tiny camera attached that’s used as a viewing system for examining areas deep inside the body—a surgeon can get a precise look at the spinal discs, herniated disc fragments, and nerve roots in the lumbar spine.
Percutaneous transforaminal endoscopic discectomy is similar to tubular discectomy in that it has a very steep learning curve due to spine surgeons having less experience with the approach than open or microdiscectomy techniques. While some speculate3 that PTED procedures result in a shorter operation time and hospital stay, no existing evidence indicates the approach is more successful than microdiscectomy.
If looked at from the amount of disc being removed during surgery, a surgeon can take an aggressive or limited approach with any of these surgical techniques, depending on the extent of the herniation and amount of loose disc material present. You can read more to learn about aggressive versus limited discectomy surgery.
Is there technology available to improve outcomes?
The most reputable spine surgeons utilize proven, emerging technologies and techniques over time to improve outcomes and perform faster, safer, more effective procedures. Recurrent disc herniation that requires a repeat discectomy surgery is a really big problem. Patients with large holes in their herniated disc, which account for around 30 percent4 of the lumbar discectomy population, have nearly a one in four chance5 (or 25 percent risk) of experiencing reherniation.
In other words, it’s essential to aim at prevention of secondary surgery (which is often less effective than the initial procedure) and explore any and all options available to do so. The Barricaid implant is a perfect example of an innovative technology designed to improve surgical results. The device, which is implanted during either open or micro (tubular) discectomy procedures, helps preserve the disc for patients with large holes. Closing large holes in a herniated lumbar disc with Barricaid can reduce reoperation risk by nearly 50 percent6.
How do I know which discectomy technique is a fit for me?
While there are advantages and disadvantages to each approach, an experienced, board-certified spine surgeon with the right qualifications can make an informed decision on the best option for relieving your pain. Consult with a physician (your primary care provider or a spine specialist) for an exam, diagnosis, and treatment plan customized to meet your specific needs.
While this blog is meant to provide you with information you need to make an informed decision about your treatment options, it is not intended to replace professional medical care or provide medical advice. If you have any questions about the Barricaid, please call or see your doctor, who is the only one qualified to diagnose and treat your spinal condition. As with any surgical procedure, you should select a doctor who is experienced in performing the specific surgery that you are considering.
If you have any questions about Barricaid, you may ask your doctor. For additional information, please visit http://www.barricaid.com. For complete risk-benefit information: http://www.barricaid.com/instructions-for-use.
References
1 George J. Dohrmann and Nassir Mansour, “Long-Term Results of Various Operations for Lumbar Disc Herniation: Analysis of Over 39,000 Patients,” Med Princ Pract 24, no.3 (2015): 285-290, doi: 10.1159/000375499.
2 Mark P. Arts, MD, et al, Tubular Diskectomy vs. Conventional Microdiskectomy for Sciatica: A Randomized Controlled Trial,” JAMA 302 no. 2 (2009): :149–158, doi: 10.1001/jama.2009.972.
3 Pravesh S. Gadjradj, MD, et al, “Percutaneous Transforaminal Endoscopic Discectomy versus Open Microdiscectomy for Lumbar Disc Herniation,” Spine (2020), doi: 10.1097/BRS.0000000000003843.
4 Larry E. Miller et al, “Association of Annular Defect Width After Lumbar Discectomy With Risk of Symptom Recurrence and Reoperation: Systematic Review and Meta-Analysis of Comparative Studies,” Spine 43, no. 5 (2018): E308-E315, doi: 10.1097/BRS.0000000000002501.
5 Ibid
6 Peter D. Klassen et al, “Post-Lumbar Discectomy Reoperations That Are Associated with Poor Clinical and Socioeconomic Outcomes Can Be Reduced through Use of a Novel Annular Closure Device: Results from a 2-Year Randomized Controlled Trial,” ClinicoEconomics and Outcomes Research 10 (2018): 349-357, doi: 10.2147/CEOR.S164129.


Comments