
Each year, approximately 1-2 percent of people1 between the ages of 30-50 experience sciatica, or pain that radiates along the sciatic nerve from the lower back down each leg. While any spinal condition that compresses nerves in the lower back can cause symptoms, lumbar disc herniation has been shown to cause around 90 percent2 of all sciatica cases.
If you’re struggling with sciatica, there’s no need to suffer in silence. Thanks to medical and technological advancements, today there are a number of nonsurgical and surgical treatments available. While some sciatica patients can manage their leg pain from a lumbar herniated disc with conservative nonsurgical treatments, others may require surgery to achieve lasting pain relief in cases of failed conservative treatment.
With that said, surgery to decompress the sciatic nerve and minimize sciatica symptoms may not be the best option for every patient; it is dependent on a number of factors from the degree of herniation to the type of symptoms. First, we will review whether surgery for sciatica is the right next step.
Treating Your Leg Pain with Lumbar Discectomy
In a discectomy surgery, the surgeon will remove the pieces of herniated disc that are putting pressure on your nerves. However, before your spine surgeon moves forward with discectomy surgery for your sciatica, they should always be willing to discuss nonsurgical treatment options and whether or not you’re a candidate for surgery.
It’s also essential your surgeon rules out any less common causes of sciatica such as piriformis syndrome, tumor, fracture, or infection before moving forward with treatment, as these conditions may require a different approach. Fortunately, physical examinations are now being matched with radiographic imaging to allow surgeons to reach a full diagnosis before determining the recommended course of treatment.
Several factors contribute to whether or not surgery for sciatica is recommended, such as:
- Severity and type of symptoms: If you’re experiencing severe leg pain (as opposed to back pain), weakness, numbness, and/or difficulty lifting the top of the foot (foot drop), you’re likely a candidate for lumbar discectomy surgery. Symptoms of related conditions like cauda equina syndrome (which causes incontinence along with sciatica symptoms) indicate a definite need for surgical treatment.
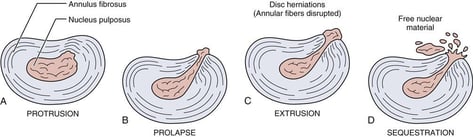
- Extent of lumbar disc herniation: The extent of your disc herniation (and whether or not sequestration, or disc fragments that break off, has occurred) is a significant factor for patients weighing surgical and nonsurgical treatment options for sciatica.3
- Condition of your lumbar spine: What is the overall condition of your spine? Your surgeon will review the condition of your bones, discs, joints, and nerves and help determine which treatment or surgery will be most effective.
- Ineffective nonsurgical treatment: Treatment guidelines dictate a certain period of conservative care (typically six weeks4) before considering surgery. If you’ve already explored more conservative treatment options, such as exercise and stretching programs, with little success, then you may be a good candidate for lumbar herniated disc surgery.
Next, we will review the different types of discectomy surgery for sciatica and the pros and cons to each approach. Lumbar discectomy is the leading surgical option for herniated disc relief. Today, many spine surgeons utilize a special type of microscope called an endoscope with the goal of improving visualization during surgery (and recovery afterwards) without the need for a larger incision.
Discectomy surgery for a lumbar herniated disc can either be aggressive or limited, depending on the amount of disc material that is removed. Aggressive discectomy involves removing all free disc fragments, as well as any additional material from inside the disc. Limited discectomy (or “sequestrectomy”) involves removing free disc fragments while preserving as much as possible of the patient’s native disc material.
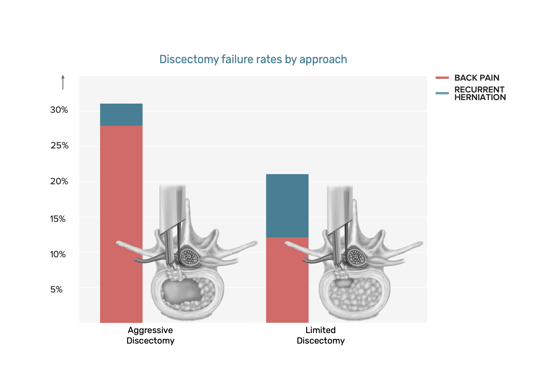
There are pros and cons to both approaches. Removing extra healthy tissue during aggressive disc removal can lead to a loss of disc height over time, disc collapse, and associated back pain. Alternatively, a limited procedure has nearly double the risk of reherniation. If you’re considering discectomy surgery for sciatica to relieve symptoms resulting from a lumbar disc herniation, a spine surgeon can explain the best procedure and approach based on the type of disc herniation you’re experiencing.
Improving Surgical Outcomes with the Barricaid Device
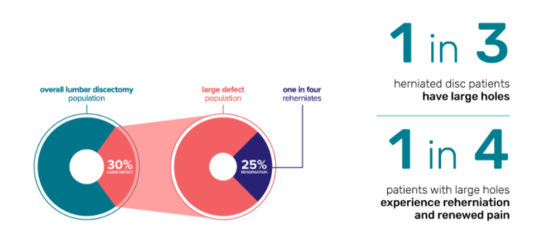
For patients with large holes (6mm wide and larger) in their lumbar herniated disc, the risk of reherniation and reoperation is all too real. In fact, patients with large holes have 2.5 times the risk5 of reherniation and 2.3 times the risk6 of reoperation compared to other discectomy patients. It’s also important to note that this 30 percent of patients makes up >70 percent of reherniations. These patients are typically treated with an aggressive discectomy procedure.
Implantation of the Barricaid device during discectomy surgery can significantly reduce reherniation and reoperation risks, because it blocks the hole where disc material could otherwise reherniate through. Barricaid is designed to withstand up to 330 pounds per square inch of pressure, or 10 times the pressure7 in a standard car tire. Ultimately, using Barricaid allows spine surgeons to perform limited lumbar discectomy surgery to maintain disc height, integrity, pressure, and function, while avoiding the risk of reherniation that usually comes with limited discectomy
The results speak for themselves: Patients with large holes present in their herniated disc saw a 50 percent reduction8 in symptomatic reherniation and reoperation after implantation of the Barricaid device. In other words, Barricaid may offer a promising solution for many patients at a higher risk of developing symptomatic reherniation.
While this blog is meant to provide you with information you need to make an informed decision about your treatment options, it is not intended to replace professional medical care or provide medical advice. If you have any questions about the Barricaid, please call or see your doctor, who is the only one qualified to diagnose and treat your spinal condition. As with any surgical procedure, you should select a doctor who is experienced in performing the specific surgery that you are considering.
If you have any questions about the Barricaid, you may ask your doctor. For additional information, please visit www.barricaid.com. For complete risk-benefit information: www.barricaid.com/instructions-for-use.
References:
1“Herniated Lumbar Disc,” Know Your Back, North American Spine Society, accessed May 17, 2020, https://www.spine.org/KnowYourBack/Conditions/Degenerative-Conditions/Herniated-Lumbar-Disc.
2Anfeng Xiang et al. “Immediate relief of herniated lumbar disc-related sciatica by ankle acupuncture: A study protocol for a randomized controlled clinical trial,” Medicine 96, vol.. 51 (2017), doi: 10.1097/MD.0000000000009191.
3Lawrence Walter Mysliwiec et al, “MSU Classification For Herniated Lumbar Discs On MRI: Toward Developing Objective Criteria For Surgical Selection,” Eur Spine J 19, no. 7 (2010): E1087-1093, doi: 10.1007/s00586-009-1274-4.
4Andrew J Schoenfeld et al, “Treatment of Lumbar Disc Herniation: Evidence-based Practice,” Int J Gen Med 3 (2010): E209-214. doi: 10.2147/ijgm.s12270.
5Larry E. Miller et al, “Association of Annular Defect Width After Lumbar Discectomy With Risk of Symptom Recurrence and Reoperation: Systematic Review and Meta-Analysis of Comparative Studies,” Spine 43, no. 5 (2018): E308-E315, doi: 10.1097/BRS.0000000000002501.
6Ibid.
7H.J. Wilke et al, “New in Vivo Measurements of Pressures in the Intervertebral Disc in Daily Life,” Spine 24, no. 8 (1999): 755-762, doi: 10.1097/00007632-199904150-00005.
8Larry E. Miller et al, “Expert Review with Meta-Analysis of Randomized and Nonrandomized Controlled Studies of Barricaid Annular Closure in Patients at High Risk for Lumbar Disc Reherniation,” Expert Rev Med Devices 17, no. 5 (2020): 461-469, doi: 10.1080/17434440.2020.1745061.


![[You may be able to decrease your chance of a repeat herniation after your first discectomy by 50%. Take this quiz to find out.]](https://no-cache.hubspot.com/cta/default/7330018/10ff7b73-96e0-4fa7-919b-f4b5430bd91b.png)
Comments